Morning sickness symptoms is a misnomer and can begin in the afternoon, the evening, morning and any in-between time you can think of. This was what my 3-year-old said to me, “Diarrhea is coming out of mommy’s mouth!”
So, when does morning sickness start? “Morning sickness often starts from 6 weeks – around two weeks after you miss your period,” explains GP Dr. Philippa Kaye.
This is a very common occurrence in the first, third to half of your pregnancy.
So basically, at the beginning.
For me personally, I had it for the first three months.
You can read my story here.
Table Of Contents
- 1 What is Morning Sickness? ALL DAY SICKNESS!
- 2 What is Hyperemesis Gravidarum?
- 3 When Does Morning Sickness Start And End?
- 4 What Does Morning Sickness Feel Like?
- 5 How Many Hours A Day Will Morning Sickness Affect Me?
- 6 The Story of Meredith Crowhurst: Veterinarian and mother of 3 happy babies 🙂
- 7 What Are The Common Triggers of Nausea and Vomiting?
- 8 Where did the term “morning sickness” come from?
- 9 What Causes Morning Sickness?
- 10 What Is The Purpose of Morning Sickness?
- 11 If I don’t have morning sickness, does that mean my pregnancy is more likely to abort?
- 12 If I Had It This Pregnancy, What Are The Chances I Will Get It Next Pregnancy?
- 13 How Do I Know If It Is Morning Sickness or Something Else?
- 14 Will Nausea Affect My Baby, My Health, My Family?
- 15 My Health
- 16 My Family
- 17 How Can I Prepare For Morning Sickness?
- 18 What Can I Do To Relieve And Get Through This?
- 19 What behavioral and dietary modifications can help?
- 20 Woman-to-Woman Help and Advice Along With Health Professionals include:
- 21 What herbal and vitamin and non-medical treatments are available?
- 22 What Medical Treatments Are Available For Morning Sickness?
- 23 Common Questions:
- 24 What Are The Most Effective Treatments for Morning Sickness?
- 25 HELP: If You Are Sick of Morning Sickness?
- 26 Is This A Normal Part Of Pregnancy? An Online Lesson On How To Prevent Morning Sickness
What is Morning Sickness? ALL DAY SICKNESS!
This refers to nausea, vomiting, and/or retching that many women have during pregnancy.
For some, it is merely a mild discomfort but for others, it amounts to a distressing, debilitating time.
There are many technical terms for morning sickness.
Amongst medical professionals, its most commonly referred to as “Nausea and Vomiting of Pregnancy” or NVP.
Some pregnant women will experience nausea only, without any vomiting.
This is what I experienced.
Extreme nausea and dry heaving.
While this may seem less severe, it can be just as, if not more, worse than vomiting.
A number of women experience retching only, where there is dry heaving but no stomach contents are brought up.
This occurs frequently enough that doctors classify retching in pregnancy as separate from vomiting.
Despite the term “morning sickness”, nausea and vomiting can occur at any time throughout the day or night.
The term is coined because it is quite common for nausea to occur shortly after waking, due to the combination of low blood sugar levels and having an empty stomach from fasting overnight.
For some women, this may be the only period of sickness during the day but many more women find it worse later in the day or at night.
Common triggers and causes of nausea and vomiting during pregnancy include:
- Having an empty tummy
- Brushing the teeth
- Smell
- Sight – I couldn’t even look or go into a grocery store.
- Taste of certain foods – which is unique to each and every individual woman.
Again, I could not stand any food cooking or people talking about food.
This can have a serious impact on the individual, the family, the workplace, and the community.
It’s the single most common reason for pregnant women needing to go to the hospital in the first half of pregnancy and it is the second most common reason for hospital admission in the second half of pregnancy, second only to premature labor [6, 19, 20].
What is Hyperemesis Gravidarum?
In a very small amount of women, vomiting in pregnancy is very severe and persistent.
This condition is referred to as hyperemesis gravidarum.
The frequent, prolonged vomiting typically causes weight loss, often more than 5% of pre-pregnancy weight.
Unbeknownst to me, some women are having abortions due to HG.
Read more here about their story HERE.
In an attempt to provide more energy for the baby, the body starts to break down and use muscle for energy.
A waste by-product of this process is ketones.
Laboratory tests often show an increase in ketones in the blood and urine.
The ketones are toxic to the body in large amounts and contribute to feeling yucky.
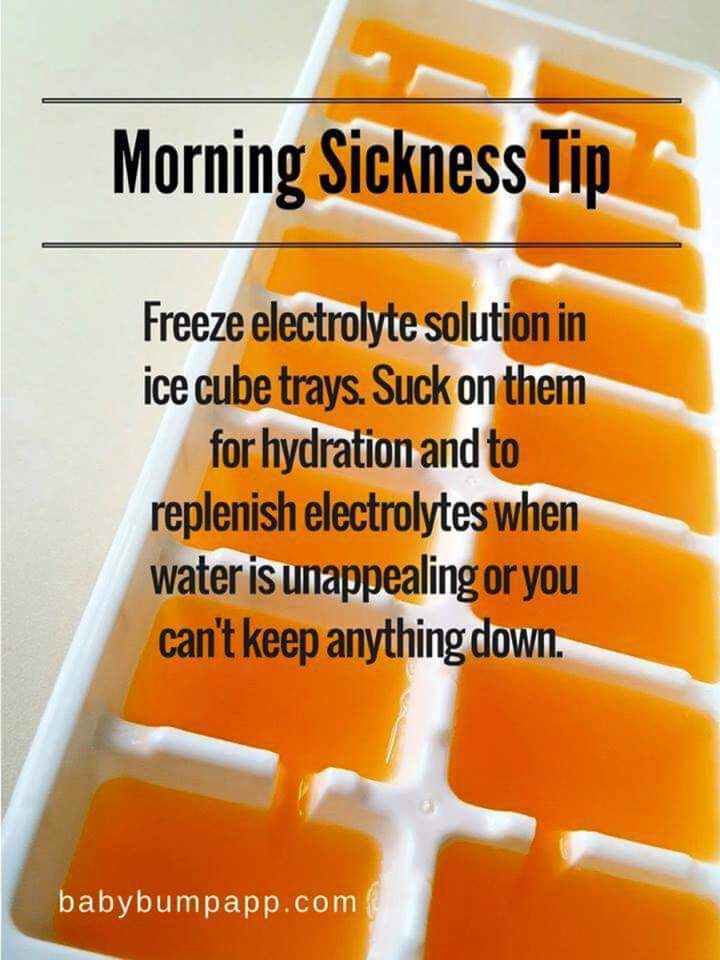
The severe and prolonged vomiting can also cause dehydration and electrolyte imbalances. Many women need to go to the hospital for treatment.
This treatment may include intravenous fluids to correct dehydration and nutritional support.
What if I just can’t keep anything down?
Early treatment may prevent progression in some cases. It can also prevent the need for hospitalization.
Women who have had HG in a previous pregnancy are at risk of having it again.
These women, in particular, should seek treatment when the first symptoms of morning sickness occur in a subsequent pregnancy. [4, 14, 22]
Diagnosis of HG is by exclusion – your healthcare provider will rule out other possible causes based on your symptoms, and will diagnose HG if nothing else fits.
HG symptoms include:
- Persistent vomiting not related to illness
- Dehydration
- Low blood pressure
- Ketones in the urine (ketones occur when your body uses fat for energy instead of glucose and is a marker of starvation.)
- Excessive weight loss
- Imbalances in electrolytes, thyroid hormones, and liver enzymes
It is estimated that from 50-80% of women get nausea during pregnancy and up to 50% have vomiting and/or retching.
Hyperemesis gravidarum is much rarer. It occurs in about 0.3-3% of women. [6, 8, 19, 25]
When Does Morning Sickness Start And End?
You mean how early can morning sickness start… well it occurs mostly in the first trimester.
It usually starts between weeks 5 and 6 of gestation (counted from the start of the last menstrual cycle) but can start as early as four weeks and usually makes its appearance suddenly.
For the majority of women, morning sickness ends at weeks 12-14 of gestation but can continue up to 20 weeks.
For an unfortunate 15-20% of women, pregnancy sickness continues past 16-20 weeks [8, 13].
Very occasionally, a woman can have nausea and vomiting for her entire pregnancy.
What Does Morning Sickness Feel Like?
Feels unlike many other types of nausea, vomiting, or retching.
There are no abdominal pain, headache, fever, or chills as you might get with nausea associated with illnesses, such as gastroenteritis.
Also, unlike other causes of nausea and vomiting, it’s often worse when the stomach is empty.
Eating small amounts can actually make nausea feel better.
I remember eating cut up white grapes with cut up Havarti cheese. (don’t ask why this particular cheese, I was just able to stomach it)
From common pregnancy forums, women have described morning sickness as similar to the nausea of a really bad hangover.
The other common comparison is of motion sickness.
It also feels very much like nausea associated with estrogen-containing contraceptive pills.
The feeling of being heavy and weighed down.
How Many Hours A Day Will Morning Sickness Affect Me?
Are some pregnant women more likely than others to feel nauseated?
About 25 % of pregnant women do not experience any nausea or vomiting [19].
Some will only be affected for a few days, while some will experience discomfort for weeks.
Nausea may affect some for only a short period throughout the day or come and go.
Some are most affected in the morning, some at night. It is highly variable for each woman and for each pregnancy.
There is no normal or “supposed to be”.
Vomiting that lasts for more than six hours during the day is considered on the more severe side [19].
If I don’t have morning sickness, does that mean I’m more likely to have a miscarriage?
No and comfort should be taken in the fact that this sickening feeling indicates a healthy functioning placenta and that, in most instances, nausea and vomiting will end around the end of the first trimester… for most anyway.
During this period, morning sickness should be viewed with sympathy and every effort should be made to help the woman get through it.
There are numerous ways in which husbands, partners, family members, and friends can help… from their understanding to providing help and allowances for altered routines and eating habits.
God forbid I smelled bacon cooking!
Having this condition does not usually harm the mother or the baby but if the vomiting is severe or prolonged, the woman should seek medical advice.
Just like pregnancy, nausea and vomiting are finite and the morning sickness will eventually end.
Click here to view more details if you want to know how to avoid morning sickness because there ARE things you can do to start feeling better now!
In her “Beautiful Babies” e-course, Kristen of Food Renegade offers these tips for managing morning sickness and food aversions while getting your baby the best nourishment possible.
The Story of Meredith Crowhurst: Veterinarian and mother of 3 happy babies 🙂
“I’ve have had three babies.
My first pregnancy: Everything was going really well. I was elated and energetic then, at five weeks gestation, nausea suddenly reared its ugly head.
It was bad from the start.
I rarely vomited but I had nausea on and off throughout the day.
I couldn’t brush my teeth properly – putting the brush anywhere near those back teeth caused me to gag and retch.
To this day, when I am brushing my teeth, I still have flashbacks to that gagging sensation.
My nausea was worse at night.
I might have predicted this.
When I was on the contraceptive pill, I had the same nausea every evening.
This was worse though. Unfortunately, this time period coincided with my training in an emergency veterinary clinic, which involved overnight shifts from 6 pm to 6 am.
Instead of sleeping through my worst time of day, I suffered from constant nausea all night.
It was exacerbated by the tiredness.
The main way I got through the night was by eating soup and whatever I could stomach, in small amounts and very frequently to avoid an empty tummy!
I also avoided the methylated spirits disinfectant bottle because that made me feel worse. I had a new aversion to coffee, hot chocolate, ham, and countless other foods, which often varied from day to day.
I ate whatever didn’t look too unappealing.
On many occasions my husband made a quick dash to the supermarket to buy my latest request when I had rejected, or worse, retched at his hard-labored meal offering.
The nausea suddenly went away at the end of week 14.
I was confined to bed for two days with gastro, which I had caught from my niece, and arose with no gastro and no more morning sickness!
My second pregnancy: I was traveling overseas in the first trimester.
Initially in France, at the start of week six, I had the hopeful thought that morning sickness might not get me this time.
Then we travelled through Abu Dhabi on the way home. Abu Dhabi is stiflingly hot and dry.
We thought it might be nice to check out the camel market, which turned out to be a holding pen for a nearby abattoir in the middle of the desert.
There was a long bus ride to the middle of nowhere.
I step out the door and with the heat and smell, I nearly threw up. From that point on the nausea continued and lasted until the end of week 16.
I don’t remember the nausea as well as my first pregnancy.
In general I think it was worse – I actually vomited more.
This was interesting because my down syndrome screening test showed by blood had higher than average levels of hCG, which might be associated with morning sickness.
I coped better with the morning sickness this time round, probably because I was better rested and knew how to control it better.
(Nothing compared to those nauseous overnight stints at the emergency clinic!) This pregnancy, the main food that was appealing and helped quell the nausea was fatty take-away food.
It wasn’t great for the waist but I would have done anything to stop feeling sick and I reasoned it was for a short period anyway.
I don’t remember as much of my third pregnancy.
The other two were girls. This was a boy. I felt different this time around. The nausea wasn’t as bad. I don’t remember when it started and I think it ended around week 12.
Looking after two toddlers, I didn’t have the time to feel sick.
I just had to keep working through it, but I think it distracted me somewhat.
The only interesting thing in this pregnancy happened once again when I was traveling.
The family took a trip to Cairns when I was about 14 weeks pregnant and my morning sickness had disappeared by then.
We went out to look at the Great Barrier Reef and hopped on a glass bottom submarine.
I usually don’t get sea sick but I suffered really badly that I had to get off the boat. I tried ginger tablets. It helped maybe slightly.
Throughout all my pregnancies, to ease my nausea, I mainly used dietary modification, rest, and exercise.
My obstetrician prescribed the anti-nausea medication metoclopramide, but I didn’t feel comfortable using it.
For me, morning sickness was one of the most unpleasant memories of the entire pregnancy and I have sympathy for any woman that suffers it for even one day.”
What Are The Common Triggers of Nausea and Vomiting?
There are many triggers of nausea and vomiting in women suffering from morning sickness.
The triggers are very individual and sometimes bizarre.
A common trigger is an empty stomach, hence the cliché of the pregnant woman vomiting first thing in the morning.
Brushing the teeth, particularly the back teeth is another common trigger.
Many women are affected by the sight, smell, and taste of particular foods.
Stronger smelling foods, caffeine, and meats are more common triggers. For me, any green veggies, bacon, eggs or everything really!
The particular foods that trigger the gag reflex are different for each woman, for every pregnancy, and even varies throughout the period of morning sickness.
Sudden changes in temperature or being overheated can make nausea worse, as can stress.
Prolonged crouching, hunching over, or lying down immediately after eating can also make nausea worse.
Some pregnant women also report that smoking or cigarette smoke makes them feel sick.
Motion sickness will be exacerbated and some women may suffer from motion sickness when they never did before.
Basically, there are many many triggers of nausea and vomiting with this condition.
Where did the term “morning sickness” come from?
It didn’t use to relate to pregnancy and wasn’t just confined to women [23].
Why do they call it morning sickness when I feel nauseated all day long?
Before the 1900s, men used to get this as well. Any nausea or vomiting that occurred in the morning, such as after a late-night drinking session.
It is only from the 1860s that the term was used to define a unique condition suffered by women in pregnancy that needed a doctors’ treatment.
At that time, the condition began appearing in the first medical journals.
Nowadays, the term is solely associated with pregnancy.
What Causes Morning Sickness?
If I don’t have morning sickness, does that mean I’m more likely to have a miscarriage?
The cause remains unknown.
It is likely there are multiple factors that play a role.
Primarily, its thought to be related to the changing levels of various hormones in the bloodstream, such as human chorionic gonadotrophin (hCG), estrogen, progesterone, and thyroid-stimulating hormone (TSH) [12, 17].
During early pregnancy, following implantation of the fertilized egg, the placenta produces a hormone called hCG.
This protein is detectable in blood and urine and is the basis of most pregnancy tests.
It is critical for the continuation of the pregnancy.
It tells the ovaries that there is a fertilized egg and to continue producing progesterone and estrogen to support a pregnancy, rather than continuing through the menstrual cycle.
Production of this hormone starts from about 9 days after fertilization and continues to rise, peaking at 7-12 weeks of gestation.
It then declines to a lower stable level for the rest of the pregnancy.
The association with morning sickness comes from the fact that peak blood hCG levels correlate with the period when this occurs [7].
Furthermore, it generally occurs more frequently and is more severe in pregnancies where there are higher levels of hCG.
This occurs when there is more placental tissue present, such as in multiple gestations (twins, triplets etc.) or with molar pregnancies (cancer-like growth of the placenta). [13]
Nausea and vomiting might not be directly caused by hCG but may be related to other hormones or factors influenced by hCG [13]. hCG causes an increase in estrogen, progesterone, and TSH levels.
Studies have shown a link between high estrogen levels and women with morning sickness.
Indeed, some women who take the estrogen-containing contraceptive pill suffer from nausea and vomiting that feels similar to morning sickness.
The degree of sickness increases with higher levels of estrogen in the “pill”.
Conversely, cigarette smoking is associated with lower hCG and lower estrogen levels and pregnant smokers are less likely to suffer from hyperemesis gravidarum [19].
Whether or not a woman gets sick and the severity may also be affected by how her individual body reacts to the hormone levels.
Genetic factors likely play a role.
Deficiencies in certain nutrients, such as vitamins B6 and B12 and potassium, may also have an influence.
Stress and tiredness also exacerbate morning sickness in many women. [13]
There are other factors that may contribute:
During pregnancy, hormones tell the stomach and intestines to slow down the passage of food so they can extract more nutrients. They also cause increased acid in the stomach and alter the metabolism of carbohydrates.
Unfortunately, a side effect is bloating and gas, which can cause discomfort and contributes to nausea.
Pregnant women can also have fluctuations in blood pressure, particularly having low blood pressure, and this may contribute.
The pregnant woman also develops a heightened sense of smell.
(I couldn’t even walk into the grocery store because of the smell) There are also a lot of changes occurring physically in the body and with the uterus.
These physical changes may contribute to feelings of nausea. [13]
Many women also report feeling sick after taking pregnancy vitamin tablets. (my prenatal pills smelled like vomit to me!) Vitamin tablets can be quite potent and can affect digestion.
Iron, for example, while important for pregnancy, can cause constipation and bloat.
Trying different brands of quality vitamin tablets, taking a vitamin that doesn’t contain iron, taking them on a full tummy, and splitting the dose throughout the day has been reported to help some.
Interestingly, there appears to be a link between Helicobacter infection and the incidence and severity of morning sickness [13].
Helicobacter is a bacteria that lives in the stomach.
It contributes to the development of stomach ulcers.
Several studies indicate there is a higher prevalence of Helicobacter infection in women with severe morning sickness and treating for Helicobacter can lessen the severity of the disease.
What Is The Purpose of Morning Sickness?
It is unknown why women get morning sickness.
There are two main theories [5].
#1. That nausea and vomiting are an unpleasant side effect of pregnancy and serve no real purpose.
#2. The other theory, the adaptation theory, proposes that morning sickness developed as a mechanism for protecting the mother and the fetus from eating foods that might be potentially harmful.
Humans are the only mammals that suffer from morning sickness.
It is argued that because we are traditionally hunter-gatherers, with a wide food base, we have evolved morning sickness to protect ourselves from harmful food choices.
To support the argument, researchers argue that the foods that commonly trigger morning sickness, such as the strong odor of rotten vegetables, coffee, ham etc. are those foods that could potentially cause harm. < This was particularly interesting to me.
If I don’t have morning sickness, does that mean my pregnancy is more likely to abort?
Studies have shown there is a lower rate of miscarriage amongst women who have morning sickness.
This is thought to be associated with the development of a robust placenta.
However, about 25% of pregnant women do not get it at all and have a normal healthy pregnancy.
If you don’t have it, this does not indicate that the pregnancy will abort.
On the other hand, you can take heart from the fact you have developed a strong placenta to support the growth of your fetus. [19]
If I Had It This Pregnancy, What Are The Chances I Will Get It Next Pregnancy?
How will I know if I will get morning sickness?
If you had pregnancy sickness with a previous birth you may not get it again, however, your risk may be higher.
The rate of recurrence in subsequent pregnancies can range from 15-81% [19].
- One study indicated two-thirds of women who had severe morning sickness will suffer from a severe form of it again in subsequent pregnancies.
- Half of the women who had mild morning sickness in a previous pregnancy suffered from it worse the next [19]. The recurrence rate for hyperemesis gravidarum is 75-85% [14].
- If you were hospitalized for severe vomiting in a previous pregnancy, there is a high risk you will need to be hospitalized again in a subsequent pregnancy [4].
- Knowing this information is important since, for hyperemesis gravidarum, there is evidence to suggest that early treatment, or even pre-emptive treatment on the first day or before symptoms begin, can reduce the severity of morning sickness and reduce the recurrence of hyperemesis gravidarum [10].
- If your biological mother or sister had morning sickness, there is a higher chance you will get it. Also, if you suffer from nausea with the contraceptive pill, there is a higher chance you will get morning sickness. There are some suggestions that carrying a female fetus, or having a history of motion sickness or migraines also increases the risk.
How Do I Know If It Is Morning Sickness or Something Else?
Morning sickness will usually first occur before week 9-10 of pregnancy.
If nausea first occurs after this time, it is advisable to see a doctor determine if there is another cause [19].
There are many causes of nausea and vomiting unrelated to pregnancy and some of these cases occur more commonly in pregnancy.
- Examples include gallstones and gall bladder disease, bladder infections, gestational diabetes, high blood pressure, and eclampsia.
- The pregnant body also has a lowered immune system, which is necessary so the body doesn’t treat the baby as foreign.
- However, this means that a pregnant woman is more prone to getting infections, such as gastroenteritis from other people or from “off” food.
Will Nausea Affect My Baby, My Health, My Family?
Morning sickness does not usually harm the baby. There is no evidence that even frequent vomiting with some weight loss harms the baby, particularly if you make up for the weight loss in later months.
Only in circumstances of severe morning sickness is the baby at risk.
The most common adverse outcomes are being small for gestational age, low birth weight, and premature birth.
Only very rarely has hyperemesis gravidarum caused the fetus to abort.
The effects are minimized if treatment is given. [19]
My Health
Only in rare circumstances, where there is very severe hyperemesis gravidarum, can the woman’s health be at risk.
Risks include vitamin B1 deficiency, which can cause neurological disabilities or even death (Wernicke encephalopathy).
Other risks include kidney or liver failure from dehydration, or rupture of the spleen, esophagus, or lungs due to forceful vomiting.
More commonly, women with severe morning sickness are affected psychologically.
They may suffer from depression and/or anxiety. In extremely rare cases, the impact is so severe that a woman will choose to terminate the pregnancy.
Longer term, hyperemesis gravidarum can lead to a longer recovery after the birth, gallbladder problems, and muscle pain. [19]
My Family
For some women, morning sickness is merely an unpleasant distraction.
For others, it can have a profound effect on day-to-day life, both physically and emotionally [13].
To get through a day with morning sickness, it is often necessary to make changes to the normal daily routine.
It may start with eating a cracker before you get out of bed, waiting to brush your teeth, or visits to the toilet to throw up.
This may make you late for work or in dropping off the children at school.
You may need to eat small frequent meals throughout the day to quell nausea or avoid certain locations, such as cafeterias or lunchrooms, to avoid the sights and smells of particular foods.
Frequent feelings of nausea can also affect the ability to concentrate.
If there are significant changes to your routine and concentration, it can make it difficult to look after older children, perform household tasks, and function to the same standard at work.
It can also affect sleep and social activities.
Consistently, studies show higher levels of discomfort, a lower quality of life, and lost time from work in women that suffer from morning sickness.
Mentally, this can cause frustration, isolation, and anxiety and/or depression. Practically, it can cause losses in income and increased medical bills.
From a population perspective, morning sickness has a modest effect on national health spending each year [13].
How Can I Prepare For Morning Sickness?
Unfortunately, not many people have sympathy for women with morning sickness, unless it is a woman who has suffered from it herself.
It is truly hard to understand how horrible it can be unless you have been through it yourself.
Studies indicate that in many instances even partners offer poor support.
You may be lucky and not be impacted much by it, however, morning sickness is so common that it would be unwise to assume that you might go through the first trimester unaffected.
It can be wise to plan ahead – to prepare for changes to the family and work routines.
The main thing is not to be too hard on yourself and anticipate that you may not be able to achieve all that you want to or perform to the same standard during this period.
What Can I Do To Relieve And Get Through This?
Pregnant women can try a range of things to help themselves through it.
There have been different remedies offered up to help with morning sickness.
However, many of these remedies have not been well tested, so we don’t know if they really work.
Many remedies are offered up from woman to woman based on what did and did not work for them.
The most important thing is that the remedy is safe for both the baby and the mother.
Again, there are many remedies that have not been well tested in terms of safety.
If you are at all unsure, it is best to consult an experienced obstetrician, midwife, doctor, nutritionist, or maternal health care worker.
The most common and effective intervention is behavioral and dietary modification – changing when and what you eat.
Other common interventions include herbal remedies. The most common and effective is ginger.
Other herbs used include chamomile, peppermint, and raspberry leaf, frequently taken as a tea. Vitamin B6 and B12 may also be beneficial.
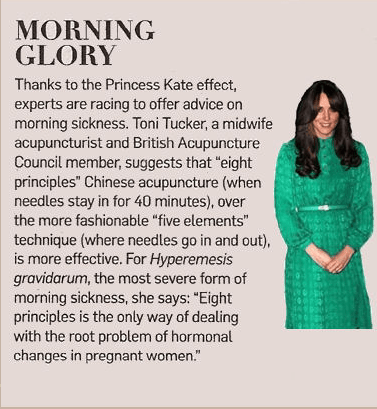
Some people have tried acupressure or wearing a pressure band (called an acustimulation band) that places constant pressure over the Neiguan point (P6), which is found on the inner aspect of the forearm, near the wrist.
Acupuncture, relaxation techniques, autogenic feedback training, hypnotherapy, and massage are also commonly tried.
For women that prefer homeopathy, the most common remedies used are Nux vomica and Pulsatilla. [14, 15, 19, 20, 21]
Certain medical drugs have also been prescribed to help treat morning sickness.
These include anti-histamines and anti-vomiting drugs.
What behavioral and dietary modifications can help?
Behavioral and dietary modification is one of the most common and effective ways to manage morning sickness [15, 19, 20].
This involves managing your eating habits and activities throughout the day to avoid triggers of nausea and find ways to settle it down.
[Here is a great post on how to stay fit during pregnancy.]
What works well for some women will not work well for others.
Many pregnant women are guided by their own bodies and, using “gut feeling” or experimentation, they find out what works best for them.
Woman-to-Woman Help and Advice Along With Health Professionals include:
- Eat small, frequent meals to avoid the stomach becoming bloated
- Eat small, frequent meals and snacks (every 1-2 hours) to avoid having an empty tummy
- Keep lots of small nutritious snacks on hand
- Eat low fat, high carbohydrate foods (toast, crackers, potatoes)
- Others advocate protein-dominant meals
- Avoid foods with strong odors and tastes
- Decrease or avoid spicy foods, if they are a trigger
- Avoid the sight, smell, and taste of foods that make you feel sick
- If solid foods won’t stay down, try liquid nutritional supplements
- Don’t be too concerned about keeping to a balanced diet for this short period
- Drink lots of fluids
- Try ice, fruit, or popsicles as a method for getting more fluids into you
- Avoid preparing and cooking food – have someone prepare it for you
- Sucking lemon drops or using mouthwash to reduce the saliva in the mouth
- Eat dry carbohydrates, such as a cracker, when you first wake up in the morning
- If vitamin capsules or tablets trigger the gag reflex, swap to chewable vitamins
- If brushing the teeth triggers the gag reflex, do so after eating rather than on an empty tummy, or go back to brushing the back teeth later in the day
- Decrease or avoid cigarette smoking
- Avoid lying down for two hours after eating
- Avoid crouching down and hunching over as this compresses the stomach
- Wear loose clothes to avoid compressing the abdomen
- Rest and relaxation exercises
I used to suck on jolly ranchers to sweet-tarts…
What herbal and vitamin and non-medical treatments are available?
A number of non-medical treatments are commonly recommended. The most common are vitamin B6, 50 mg up to and not exceeding 200 mg per day, but only on your doctor’s advice.
Also ginger, up to1000 mg/day, as tea, tablets, or in food.
Acupressure wrist bands are used for seasickness and many women use them for morning sickness as well.
They place pressure on acupoint P6, on the inside of the arm near the wrist.
While there is not much evidence that other remedies work…
Other common advice involves:
- sucking on a slice of lemon and
- taking chamomile
- raspberry leaf
- peppermint, as a tea or supplement
Some people have tried acupressure, acupuncture, hypnotherapy, and massage. [14, 15, 19, 20, 21]
What Medical Treatments Are Available For Morning Sickness?
Many women can manage morning sickness by diet and lifestyle changes alone but these are not effective for everyone.
Many people naturally have concerns about using medication during pregnancy, particularly following what happened with thalidomide.
Thalidomide: Used as a drug to treat morning sickness in the late 1950s and early 1960s, resulted in many babies born with birth defects.
Use of the drug in pregnancy occurred because, at that time, drug companies were not required to prove a drug was safe for the developing fetus.
It was assumed drugs did not cross the placenta from the mother to the fetus.
The devastating impact of the drug led to major changes in drug testing and approval in developed countries to ensure the same situation never happens again.
The memory of this event means that doctors are much more careful at prescribing any medications to pregnant and breastfeeding women.
The only safest meds I took was Tylenol for aches and colds.
Common Questions:
- What about anti-nausea medications?
- Which medications can I take for morning sickness during pregnancy?
Medications that are sometimes prescribed to help with morning sickness include:
- Antihistamines
- Metoclopramide
- Antacids
- Antibiotics to treat Helicobacter pylori infection
- Phenothiazines
- Ondansetron – there is some concern it may affect the fetus
In April 2013, the US Drug and Food Administration approved doxylamine succinate (at 10 mg/kg) as a drug to specifically treat morning sickness.
It is the first drug approved for such a purpose in more than 30 years and is intended for women whose morning sickness does not respond to other conservative management.
It is a type of antihistamine, most of which work on the part of the brain involved in feelings of nausea.
The specific medication prescribed is called Diclegis® (USA) or Diclectin® (Canada).
It is a mixture of doxylamine succinate and pyridoxine hydrochloride (vitamin B6) in a delayed-release tablet.
A good scientific study (randomized, double-blind, placebo-controlled study) has shown the drug is effective at reducing nausea and vomiting during pregnancy.
The drug is classified as a Risk Factor A drug, meaning that studies have found no detrimental effects on the fetus.
The most common side effect is sleepiness. [9, 15, 17, 19, 20]
Any medications need to be taken under complete medical supervision. Many drugs and supplements should not be taken in combination.
Therefore, it is very important that the doctor is aware of all the other herbs, vitamin, and medications that you are taking.
What Are The Most Effective Treatments for Morning Sickness?
Recent Studies:
A couple of recent reports critically reviewed all the latest scientific evidence available for common morning sickness remedies.
They were assessing both effectiveness and safety.
A 2015 Cochrane review examined the evidence from 44 clinical studies involving 5449 pregnant women.
The studies looked at the effectiveness of:
- acupressure or acustimulation
- acupuncture
- ginger
- chamomile
- lemon oil
- mint oil
- vitamin B6
- several anti-vomiting medications. [15]
The Conclusions:
- The conclusions based on the studies available were:
- Acupuncture showed no significant benefit
- Ginger may be beneficial but the evidence is limited and inconsistent
- There is limited evidence for the benefit of anti-vomiting medications, including the doxylamine-vitamin B6 combination
Another review came to the following conclusions –
There was “good and consistent scientific evidence” that the following helps reduce the occurrence and severity of morning sickness:
- Taking prenatal vitamins in the three months leading up to pregnancy
- Taking vitamin B6 or a combination of B6 and doxylamine is safe and effective. [19,20]
There was “limited or inconsistent scientific evidence” to support that:
- Ginger might have beneficial effects
- Early treatment of nausea and vomiting can help prevent progression to the more severe hyperemesis gravidarum
Basically, there is not enough high-quality evidence available in support of many of the interventions.
There are many women that swear by particular morning sickness remedies and advice has been passed down from generation to generation.
Women should try whatever they feel comfortable with as long as the remedy does not cause harm to them or their baby.
That queasy feeling in your stomach often starts when the sun rises, it can hit at any time of the day or night.
I gathered many more helpful remedies from forums:
1. Drinking the No To Morning Sickness Tea < Fan Favorite!
2. Drinking peppermint tea sweetened with a little bit of honey < great to calm your tummy
3. A reader has confirmed the following with nutritional scientists as well as midwives who can give anecdotal evidence.
“OBs do not study nutrition, but instead parrot to you what they have been told.
To study nutrition is to be a nutritionist. And that is money and time 99% of them do not have.)
If you take in empty calories and toxins (in your environment as well as your food), you will be more likely to have morning sickness.
All toxins built up over the years in your body will be mobilized when you become pregnant.
The heavy metals that are transferred to the first born are frightening.
If you lived an unhealthy lifestyle, detox safely before pregnancy.
Once you are pregnant, if your prenatal vitamins make you sick, obviously there is a problem.
A synthetic vitamin with contaminants that is over processed is not what it takes to make a healthy baby.
Check out your brand. I use Shaklee.
My pregnant friends who switched stopped getting sick.
Protein is vital. Find a form you can tolerate.”
4. The solution to nausea is simple:
- Eat Legumes/Dried Beans
- black beans
- adzuki
- fava
- pinto
- garbanzo/chickpeas
- great northern
- navy
- small red
- kidney
- lima
- butter
- cannellini
- lentils
- green split peas
- yellow split peas
- black-eyed peas
After 20 minutes of eating legumes, you should have relief.
When eating them from a can, rinse them very well.
If preparing them yourself by sorting and soaking, rinse very well after sorting, and soaking, and cooking.
Legumes are the best source of soluble fiber which binds to your bile which holds the fat-soluble hormone hCG and then is excreted from the body in your stools.
Legumes are also packed with nutrients.
They are an excellent source of potassium, iron, folate, calcium, magnesium, phosphorus, manganese, copper, and zinc.
They are an excellent source of both insoluble and soluble dietary fibers.
5. Honest brand prenatal pills
6. Diphenhydramine
7. Suck and chew slowly little bites of the apple. The pectin helps your upset stomach and the natural sugars help your blood sugar so you don’t feel so under the weather. I keep saltines by the bed to start on as soon as I wake up then I grab my apple as soon as I can after I’m up. I will cut it up into small slivers and keep them with me all day in a little Baggie. It has really helped. That and chewing half a piece of gum. The peppermint and sugars help.
8. 8oz of cold water with a tablespoon of lemon juice helps.
9. Pineapple
10. Sniffing lemon
11. Mommy’s Bliss morning sickness magic and extra Vitamin b-6 plus 1/2 tablet of Unisom at bedtime.
12. Sugared ginger helps curb the nausea
Great Article For Recipes For Nausea:
- Eating Well When You’re Too Nauseated to Eat
There are medical interventions available and if basic behavioral and nutritional modifications do not work, pregnant women should seek advice from a healthcare professional.
View this article in Glow magazine: “I couldn’t even keep a sip of water down!”
HELP: If You Are Sick of Morning Sickness?
Get support from the Motherisk Nausea and Vomiting of Pregnancy (NVP) Helpline: 1-800-436-8477
Is This A Normal Part Of Pregnancy? An Online Lesson On How To Prevent Morning Sickness
Beautiful Babies E-Course By: Kristen Michaelis, mother of three and a nutrition & wellness coach.
This course challenges common myths about “inevitable” pregnancy woes (morning sickness, stretch marks, swollen ankles, etc.) and teaches mamas how to increase fertility, have a happier pregnancy and birth a gorgeous, healthy baby.
References:
1. Einarson, A, Maltepe, C, Boskovic, R, and Koren, G. “Treatment of nausea and vomiting in pregnancy: an updated algorithm.” Canadian Family Physician, 2007; 53(12):2109-11.
2. Einarson, TR, Piwko, C, and Koren, G. “Quantifying the global rates of nausea and vomiting in pregnancy: a meta-analysis.” Journal of Population Therapeutics and Clinical Pharmacology, 2013; 20(2):e184-92.
3. Fantasia, HC. “A new pharmacologic treatment for nausea and vomiting of pregnancy.” Nursing for Women’s Health, 2014; 18(1):73-7.
4. Fell, DB, Dodds, L, Joseph, KS, Allen, VM, and Butler, B. “Risk factors for hyperemesis gravidarum requiring hospital admission during pregnancy.” Obstetrics and Gynecology, 2006; 107(2, Pt1):277-84.
5. Flaxman, SM, and Sherman, PW. “Morning sickness: adaptive causes or non-adaptive consequences of embryo viability?” American Naturalist, 2008; 172(1):54-62.
6. Gazmararian, JA, Petersen, R, Jamieson, DJ, Schild, L, Adams, MM, Deshpande, AD, Franks, AL. “Hospitalizations during pregnancy among managed care enrollees.” Obstetrics and Gynecology, 2002; 100(1):94-100.
7. Goodwin, TM. “Nausea and vomiting of pregnancy: an obstetric syndrome.” American Journal of Obstetrics and Gynecology, 2002; 186(5 Suppl understanding):S184-9.
8. Jewell, D. “Nausea and vomiting in early pregnancy.” Clinical Evidence, 2003; 9:1561-70.
9. Koren, G, Clark, S, Hankins, GD, Caritis, SN, Miodovnik, M, Umans, JG, and Mattison, DR. “Effectiveness or delayed-release doxylamine and pyridoxine for nausea and vomiting of pregnancy: a randomized placebo controlled trial.” American Journal of Obstetrics and Gynecology, 2010; 203(6):571.e1-7.
10. Koren, G, and Maltepe, C. “Pre-emptive therapy for severe nausea and vomiting of pregnancy and hyperemesis gravidarum.” Journal of Obstetrics and Gynaecology, 2004; 24(5):530-5.
11. Kramer, L, Bowen, A, Stewart, N, and Muhajarine, N. “Nausea and vomiting of pregnancy: prevalence, severity, and relation to psychosocial health.” MCN American Journal of Maternal Child Nursing, 2013; 38(1):21-7.
12. Lee, NM, and Saha, S. “Nausea and vomiting of pregnancy.” Gastroenterology Clinics of North America, 2011; 40(20):309-34.
13. Maltepe, C. “Surviving morning sickness successfully: from patient’s perception to rational management.” Journal of Population Therapeutics and Clinical Pharmacology, 2014; 21(3):e555-64.
14. Maltepe, C, and Koren, G. “The management of nausea and vomiting of pregnancy and hyperemesis gravidarum: a 2103 update.” Journal of Population Therapeutics and Clinical Pharmacology, 2013; 20(2):e171-83
15. Matthews A, Haas DM, O’Mathúna DP, Dowswell T. “Interventions for nausea and vomiting in early pregnancy.” Cochrane Database of Systematic Reviews, 2015; 9:CD007575.
16. Munch, S, Korst, LM, Hernandez, GD, Romero, R, Goodwin, TM. “Health-related quality of life in women with nausea and vomiting of pregnancy: the importance of psychosocial context.” Journal of Perinatology, 2011; 31(1):10-20.
17. Niebyl, JR, and Briggs, GG. “The pharmacologic management of nausea and vomiting of pregnancy.” Journal of Family Practice, 2014; 63(2 Suppl):S31-7.
18. Niemeijer, MN, Grooten, IJ, Vos, N, Bais, JMJ, Van der Post, JA, Mol, BW, Roseboom, TJ, Leeflang, MMG, and Painter, RC. “Diagnostic markers for hyperemesis gravidarum: a systematic review and meta-analysis.” American Journal of Obstetrics and Gynecology, 2014; 211(2):150.e1-15.
19. No authors listed. “Practice bulletin no.153: Nausea and vomiting of pregnancy.” Obstetrics and Gynecology, 2015; 126(3):e12-24.
20. No authors listed. “Practice bulletin summary no.153: Nausea and vomiting of pregnancy.” Obstetrics and Gynecology, 2015; 126(3):687-8.
21. Smith, C, Crowther, C, Wilson, K, Hothman, N, and McMillan, V. “A randomised controlled trial of ginger to treat nausea and vomiting in pregnancy.” Obstetrics and Gynecology, 2004; 103(4):639-45.
22. Sonkusare, S. “The clinical management of hyperemesis gravidarum.” Archives of Gynecology and Obstetrics, 2011; 283(6):1183-92.
23. The Lancet London: A Journal of British and Foreign Medicine, Surgery, Obstetrics, Physiology, Chemistry, Pharmacology, Public Health, and News. 1968; 1:268.
24. Viljoen, E, Visser, J, Koen, N, and Musekiwa, A. “A systematic review and meta-analysis of the effect and safety of ginger in the treatment of pregnancy-associated nausea and vomiting.” Nutrition Journal, 2014; 19:13-20.
25. Woolhouse, M. “Complimentary medicine for pregnancy complications.” Australian Family Physician, 2006; 35(9):695.










[…] Weeks Pregnant (November 3, 2014) – I feel completely exhausted. I feel totally nauseous (all day everyday). I have now stopped wearing a bra. I use black hair ties to hold my pants on. […]